In Vitro Fertilization (IVF)
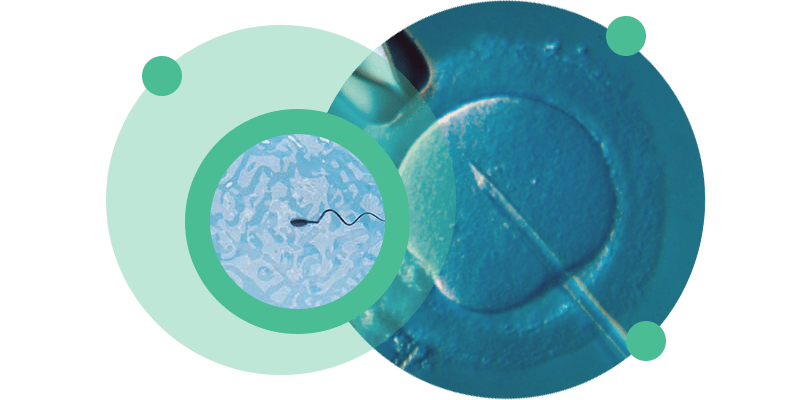
In Vitro Fertilization (IVF) is a Medically Assisted Reproduction technique in which sperm and oocytes are joined together in a laboratory environment.
IVF is indicated in cases of female infertility (such as tubal obstruction, endometriosis, ovulatory dysfunction), in cases of moderate male infertility, failures in intrauterine insemination cycles and in cases of unexplained infertility.
About In Vitro Fertilization (IVF)
In vitro fertilization is a medically assisted reproduction technique in which sperm and oocytes are combined after processing the gametes in a laboratory setting. However, this technique is based on the principles and processes that occur naturally in a woman’s body when fertilization occurs .
Naturally, during each menstrual cycle, several follicles present in the woman’s ovary are recruited by hormonal action. All of these follicles grow, but only one will be able to reach maturity – the dominant follicle – and give rise to ovulation; the rest will undergo a process of atresia. During ovulation, also triggered hormonally, an oocyte in a fertilizable state, which we call a mature oocyte, is released from the follicle and captured by the fallopian tubes. The mature oocyte comes into contact with the sperm while still in the fallopian tube and fertilization occurs. From the fusion of the female and male nuclei we obtain the embryo, a new genetic entity that will develop through successive cell divisions while continuing its journey through the fallopian tube to the uterine cavity, reaching an advanced stage of cellular differentiation – the Blastocyst – on the 5th or 6th day after fertilization. The blastocyst has the ability to attach itself to the endometrium, the layer of the uterus that allows implantation and which has also undergone changes throughout this process. If there is this synchrony between the embryo and the endometrium, implantation and subsequent pregnancy can occur.
Knowledge of the process that occurs naturally has enabled the development of medically assisted procreation techniques, such as IVF, which allows us to overcome situations in which one or more points in the process present some dysfunction.
The In Vitro Fertilization technique can be performed with gametes from both partners (in the case of heterosexual couples) or using donated gametes, whether oocytes, sperm or both.
In Vitro Fertilization is indicated in the following situations:
- female infertility
- obstruction or dysfunction of the fallopian tubes
- endometriosis
- ovulatory dysfunctions (such as polycystic ovaries, for example)
- moderate male infertility (such as moderate oligozoospermia – i.e. low sperm concentration in the ejaculate)
- unexplained infertility
- failures in previous Intrauterine Insemination cycles
Although each case is treated individually and in a personalized way by our clinical team, we present here the general stages of an In Vitro Fertilization treatment.
Ovarian stimulation
After a medical consultation and definition of the best protocol to follow, the woman’s ovaries begin to be stimulated from the 2nd day of her menstrual period. Stimulation is done using injectable hormonal medication that stimulates the growth of several follicles simultaneously, unlike the natural cycle in which, as a rule, only one reaches the necessary development for fertilization to occur. The medication used can be administered by the woman herself, at home.
After starting the medication, the growth of the follicles is monitored by ultrasound scans performed at intervals of approximately 3 days. When a reasonable number of follicles are in the pre-ovulatory stage (dimensions greater than 17 mm on ultrasound), another hormonal medication (hCG) is administered which will cause the final maturation of the follicles and the oocytes contained in them, as would happen in a natural cycle.
Follicular puncture
36 hours after taking the hCG hormone, follicular puncture is performed. This is a quick surgical procedure, performed vaginally and under sedation, during which the fluid from the follicles is aspirated using a needle controlled by ultrasound.
From this day onwards, according to the defined protocol, you can start taking new medications (orally or vaginally) that will make the uterus more receptive to receiving the embryos and allowing their implantation.
Gamete processing
The follicular fluid arrives at the laboratory and the presence of oocytes is observed. These oocytes are collected and kept in culture in incubators with a suitable atmosphere and in specific culture media.
On the same day as the follicular puncture and at around the same time, an ejaculate sample must be collected by masturbation. The sample can be collected at the clinic or at home, provided that the sample is delivered to the clinic by the patient. The ejaculate sample is processed using appropriate means that promote the selection of sperm with normal morphology and motility. The processing of cryopreserved ejaculate samples follows the same principles as the processing of “fresh” ejaculate samples.
IVF
Sperm merge with oocytes. Capable sperm will travel to the oocyte and attach to the layer surrounding it, the zona pellucida. Under normal circumstances, only one will pass through this layer and fertilize the oocyte.
Fertilization and embryo culture
16 to 18 hours after insemination of the oocytes with sperm, fertilization is observed through the presence of two pronuclei (one female and one male) that will fuse in the following hours and give rise to embryos, through successive cell divisions. The embryos remain in culture in incubators with the appropriate atmosphere and in culture media that promote their development. The development of the embryos is assessed daily.
Embryo transfer and/or cryopreservation
3 to 5 days after IVF, the best quality embryo(s) are transferred to the patient’s uterus. Embryo transfer is a quick procedure that does not require analgesia/sedation, in which one or more embryos are introduced into the uterine cavity using a catheter specifically designed for this purpose.
If it is not possible to transfer embryos in the cycle in which they were created (due to the risk of Ovarian Hyperstimulation Syndrome or another reason) or if there are more good quality embryos than can be transferred, these embryos are cryopreservated.
bHCG analysis
12 days after embryo transfer, a blood test is performed to detect the hormone bHCG, the pregnancy hormone.
IVF success rates, nationally and internationally, are around 30%.
The success rate is influenced by a variety of factors, the most important being the woman’s age, egg quality and sperm quality, so you should discuss your particular case with your doctor.






Frequently Asked Questions
Considering all stages of the treatment, including the time spent on ovarian stimulation, and even the transfer of embryos to the uterus, the time elapsed varies between 15 and 20 days.
Ovarian stimulation takes, on average, 8 to 15 days. The duration depends on the protocol used and the specific ovarian response of each woman.
The woman’s age influences the success of the technique in terms of both quantity and quality of the oocytes collected. It is known that female reproductive potential decreases significantly after the age of 35 and drops sharply after the age of 40. From this age onwards, it is more likely that the oocytes may be affected by chromosomal anomalies that negatively influence the fertilization rate and embryonic development.
It is recommended to rest for two days, abstain from sex for 5 days and avoid intense physical exertion until the pregnancy test is performed (12 days after the transfer).
The treatment does not cause pain, only some discomfort on the day the ovarian puncture is performed to collect the oocytes. The follicular puncture procedure itself does not cause any discomfort, as it is performed under sedation.
The most significant risk, which occurs in rare cases, is ovarian hyperstimulation, which will subsequently require appropriate care, but which will usually resolve spontaneously with due monitoring. Close ultrasound monitoring after the start of ovarian stimulation can significantly reduce the occurrence of these situations.
After starting treatment, the patient will have to go to the clinic every 2 or 3 days to undergo ultrasound monitoring of ovarian stimulation and, on average, 2 to 4 ultrasounds are performed until the follicular puncture is scheduled.
On the day of the follicular puncture, the husband/partner will also have to go to the clinic to have the ejaculate collected, unless he already has cryopreserved sperm or testicular tissue.
Ejaculate collection can be performed at home, provided that it is possible for the individual to deliver the sample to the clinic premises 30 to 45 minutes after collection. During transport, the container with the sample should be kept close to the body to avoid large temperature fluctuations. The collection container can be provided by CETI or a urine collection container can be purchased at any pharmacy.
You can consult CETI’s price list here.
