Testicular Biopsy (TESE)
Testicular biopsy is a minimally invasive surgical procedure performed during assisted reproduction treatments. Also known as TESE (Testicular Sperm Extraction), this technique obtains sperm directly from the testicle, for use in an in vitro fertilization (IVF) procedure using the intracytoplasmic sperm injection (ICSI) methodology.
Thus, testicular biopsy (TESE) involves the surgical removal of one or more small portions of testicular tissue, and any viable sperm observed in the tissue is extracted for use in medically assisted procreation. TESE is generally recommended for patients in whom sperm cannot be obtained by ejaculation due to azoospermia.
Azoospermia is defined as the condition in which a man's ejaculate contains no sperm. It is associated with male infertility, but some forms are amenable to medical treatment. Azoospermia affects around 1% of the male population, and can occur in up to 20% of male infertility cases.

About testicular biopsy
In 50% of childless couples, there is a factor associated with male infertility, usually associated with abnormal sperm parameters. Therefore, in all infertile couples, the man should be evaluated by a urologist specialized in male reproduction (andrology differentiation), with spermograms being the laboratory diagnostic tool initially recommended.
Testicular biopsy is a minimally invasive surgical procedure performed during assisted reproduction treatments. Also known as TESE (Testicular Sperm Extraction), this technique makes it possible to obtain sperm directly from the testicle, for use in an in vitro fertilization (IVF) procedure using the intracytoplasmic sperm injection (ICSI) methodology.
This technique, which allows direct access to testicular tissue, makes it possible to alleviate several situations in which it is not possible to obtain spermatozoa in the ejaculate, or when they are few in number and/or of poor overall quality in terms of vitality. This is particularly true of spermatozoa, motility and morphology, among other characteristics. Depending on the particular circumstances of each case, it may be necessary to surgically remove one or more fragments of tissue from one or both testicles.
Testicular biopsy (TESE) is generally recommended in patients who have no sperm present in the ejaculate (azoospermia) or who are unable to ejaculate. In general, azoospermia can be divided into two categories (obstructive and non-obstructive).
Testicular biopsy is mainly used in non-obstructive azoospermia, in which patients have no sperm present in the ejaculate, but can produce sperm in the testes and it is our duty to search for and store these sperm by testicular biopsy.
Azoospermia can be the result of genetic causes such as the presence of Y chromosome microdeletions, certain oncological situations such as testicular cancer, and certain endocrinological diseases linked to disorders of the pituitary gland or hypothalamus, responsible for regulating sperm production. Moreover, if azoospermia is linked to a disorder of sexual development, such as Klinefelter’s syndrome, characterized by the presence of an altered number of sex chromosomes, TESE can also be used to obtain sperm, as well as in other situations of great severity. TESE can also be used to obtain sperm in other serious situations, such as bilateral cryptorchidism or non-reversible azoospermia following oncological treatments.
On the other hand, testicular biopsy (TESE) can be used to extract spermatozoa in cases of obstructive azoospermia. Obstructive azoospermia can be caused by a number of factors, such as vasectomy, infection and/or trauma to the seminal tract with severe fibrosis, as well as congenital absence of the vas deferens in cystic fibrosis or otherwise.
TESE can also be used as a fertility preservation option in patients who have undergone sex reassignment surgery and are unable to ejaculate.
Spermatogenesis in the testes can be focal, meaning sperm can be found in small, isolated foci. With some variability between techniques, the sperm collection rate reaches 50% in patients with non-obstructive azoospermia.
Numerous factors predictive of positive sperm recovery have been studied, but it has not yet been possible to unequivocally demonstrate a definitive factor predictive of sperm recovery. TESE-ICSI represents a major advance in the treatment of infertility in men with non-obstructive azoospermia, with almost 4 out of 10 couples (37%) undergoing TESE-ICSI achieving delivery.
Testicular biopsy (TESE) is a minimally invasive procedure that can be performed under local anesthesia or intravenous sedation on an outpatient basis, without the need for hospitalization. In our Center, we usually use intravenous sedation, as it allows wider manipulation of the testicle, overcoming possible anatomical variations in testicular positioning, as well as the existence of previous testicular surgery, which can make local anesthesia difficult.
In this way, we always have an anesthetist present to monitor the entire procedure. The patient must fast for 6 hours and be accompanied, as he or she will not be able to drive after intravenous sedation. After obtaining informed consent, the procedure begins by shaving the scrotum, disinfecting the area with povidone-iodine and placing a sterile field.
Le testicule est fixé manuellement et une petite anesthésie locale est appliquée sur le scrotum, suivie d’une incision d’environ 1 cm dans les différentes couches de la paroi scrotale jusqu’à atteindre l’albuginée testiculaire. Ensuite, à l’aide du scalpel, une très petite incision est ouverte dans la tunique albuginée pour exposer la pulpe testiculaire.
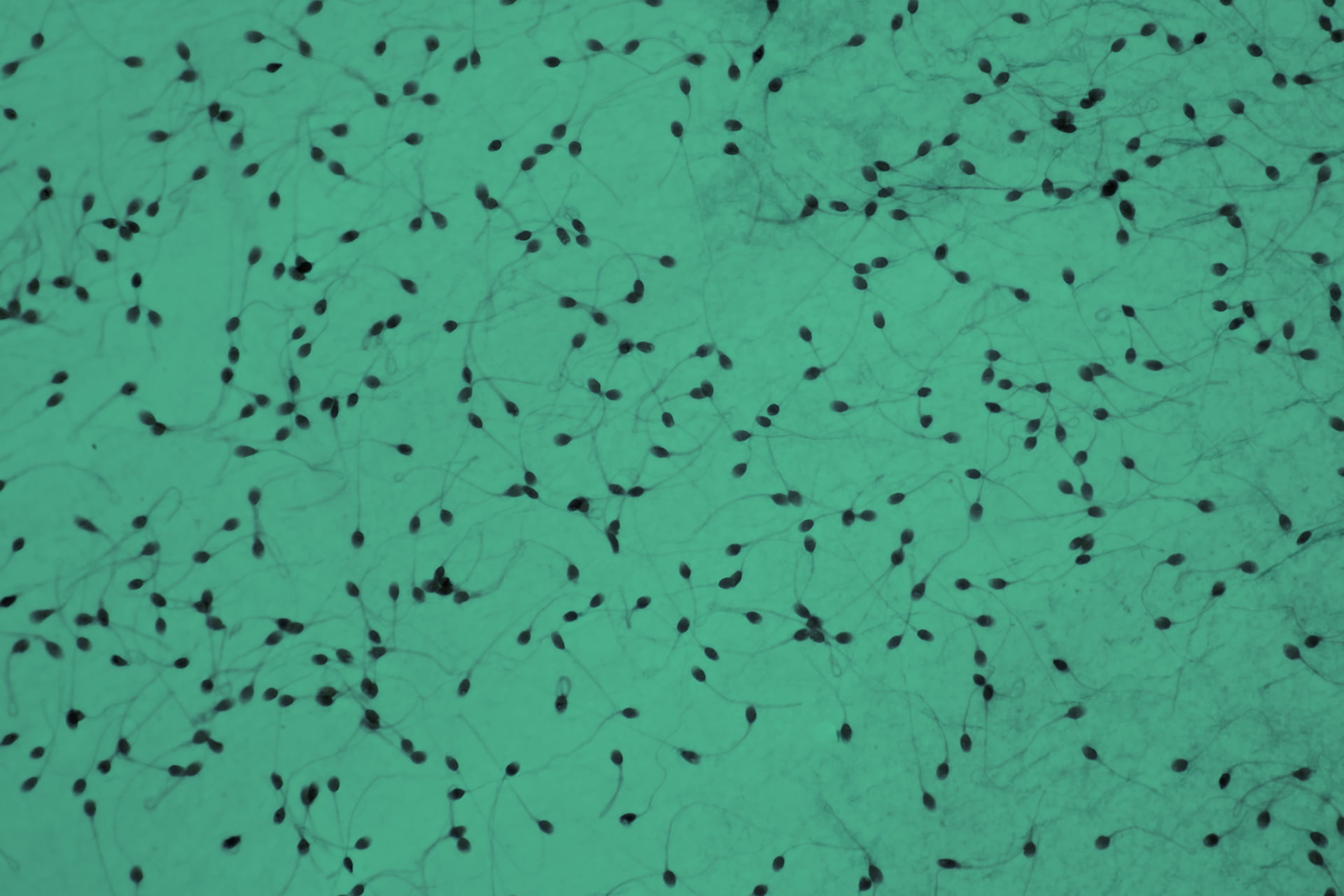
Using delicate scissors, one or more fragments of this pulp are removed and placed in a Petri dish filled with a suitable culture medium and immediately sent to the biologist who will process these samples and observe them under the microscope. If sperm of acceptable quality and in sufficient quantity are observed, they can be cryopreserved or used directly to fertilize the woman’s oocytes extracted by ovarian puncture during assisted reproduction treatments.
The procedure therefore ends here, closing the albuginea and suturing all previously open scrotal layers. If no sperm is found, the whole procedure will be repeated on the contralateral testicle, if there are no other impediments.
After healing and before discharge (always accompanied), instructions are given on how to maintain the dressing, as well as a prescription for an anti-inflammatory analgesic. If warranted, an antibiotic may also be prescribed.
As with any surgical procedure, even minimally invasive, testicular biopsy (TESE) carries a risk of postoperative infection, bleeding and pain (local discomfort). In certain rare situations, testicular biopsy can lead to rare tissue healing phenomena, which can result in testicular fibrosis and inflammation, potentially reducing testicular function and causing testicular atrophy.
In addition, in rare situations, the procedure may alter the endocrine function of the testes, causing a drop in serum testosterone levels, which may lead to a testosterone deficiency syndrome (hypogonadism). This can lead to side effects including muscle weakness, reduced sexual function, anxiety and cognitive changes.
Blood supply to the testicle may also be altered during this procedure, potentially reducing this supply. If TESE has to be repeated due to insufficient sperm recovery, patients are generally advised to wait 6-12 months to allow adequate testicular healing before further surgery.
There are no special precautions, apart from bandaging the wound until it is completely healed. Sutures generally fall out after 10 days. It is advisable to rest for 12 hours after discharge. Violent exertion is also discouraged for the first 48 hours.
Sexual activity is generally resumed between the 2nd and 3rd day after surgery. It is advisable to be alert to situations of heavy bleeding or violent pain, as well as pronounced swelling of the scrotum and/or fever, which may indicate the presence of an infection. In these situations, the CETI should be contacted.
No. This is a simple procedure performed under anesthesia. Post-operatively, some local discomfort is to be expected, easily alleviated by an anti-inflammatory analgesic for a few days.




Frequently asked questions
The procedure is quick and easy. Typically, and depending on the number of testicular pulp samples taken, and the time required by the biologist to process the samples, 20 to 30 minutes are required. If it is necessary to approach the contralateral testicle, the procedure can be extended up to 45 m. Recovery time is rapid. After about 2 hours’ recovery, the patient is discharged, with 12 hours’ rest suggested, and resumes normal life after about 48 hours.
With some variability between techniques, the sperm collection rate reaches 50% in patients with non-obstructive azoospermia. Numerous factors predictive of positive sperm recovery have been studied, but it has not yet been possible to unequivocally demonstrate a definitive factor predictive of sperm recovery. Naturally, in situations of obstructive azoospermia, this technique has a collection efficiency of virtually 100%.
In just a few days, you can return your life to 100% normal. As a general measure after any human reproductive treatment, whose every stage is fraught with strong emotions, it’s advisable to lead as regulated a life as possible. We recommend a balanced diet, avoiding tobacco and alcohol, getting a good night’s sleep, avoiding high-impact sporting activities and being aware that whatever is done is done well. It’s important to manage this notion of mind-body connection in order to realize a long-awaited dream.
No. This procedure does not affect sexual function, with the exception of situations in which testosterone production is damaged, which are very rare. Sexual activity can resume approximately 2 days after the procedure. Occasionally, there may be a certain amount of sexual inhibition, given the strong emotional charge of all these assisted reproduction procedures, which are generally overcome naturally.
In men, vasectomy results in the interruption of the vas deferens, preventing the presence of sperm in the ejaculate. Depending on the number of years following surgery, techniques to recanalize the vas deferens can be successfully performed, but in the vast majority of cases, due to multiple factors related to the couple, the simple testicular biopsy technique is more recommended, with which we can obtain sperm to produce embryos with the woman’s oocytes through the ICSI procedure.
You can consult the CETI price list here.
